About Fibralign
Company Overview

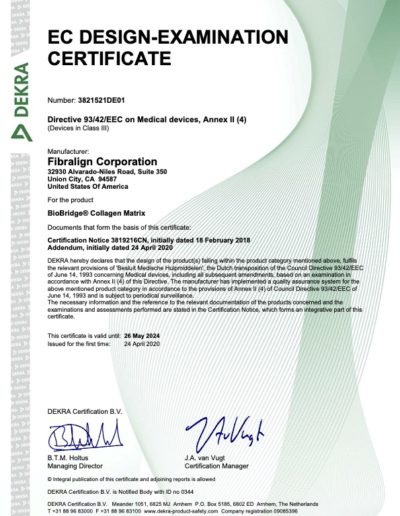
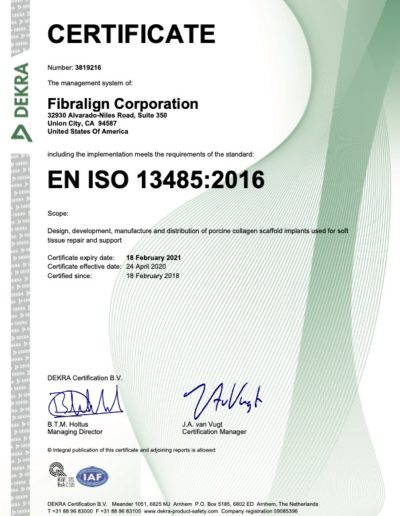
Fibralign is an award-winning, commercial-stage, Stanford-spinout that designs, develops and produces novel therapeutic medical devices to address major unmet medical needs. Based in the San Francisco Bay Area, the company’s team has established GMP commercial production (ISO 13485:2016 certified), quality system and development labs co-located at its main facility (Union City, CA).
Fibralign is supported in its mission by meaningful collaborations with leading research universities, renowned medical leaders and strategic partnerships. These relationships have proven invaluable in advancing research and development, resulting in a compelling pipeline of novel products that are based on Fibralign’s proprietary Nanoweave® scaffolding platform.
Privately held, Fibralign has been able to accomplish this progression with the support of investors and grant funding from the Department of Defense, National Institutes of Health and the National Science Foundation.
Fibralign is currently conducting a multi-site clinical study for breast cancer-related acquired lymphedema ($3M funding from the National Cancer Institute) and a pilot clinical study in Europe for the prevention of lymphedema (sponsored by Terumo Corporation). Working together with Terumo, the company is also preparing for a clinical study to be conducted in Japan in 2021 that will be used for PMDA regulatory engagement (Terumo funded).
Fibralign won the prestigious Medtech Innovator Award, taking first out of over 300 startups that participated in this annual competition. The team has maintained a strong relationship with its Stanford roots, working closely with several research groups in preclinical and clinical studies and as an active member of the Stanford StartX community. Fibralign is also an alumnus of JLABS , having been selected to join in the initial cohort of startup members for its South San Francisco location (JLABS@SSF).
Nanoweave® Technology

Fibralign’s patented Nanoweave® technology provides the means to induce self-assembly of molecular type I collagen to replicate native tissue scaffold outside of the body. This fundamental breakthrough enables medical grade collagen to be precisely printed with nanoscale features that mimic human tissue – to such a degree that the body’s tissue will interact with it naturally and not reject or challenge it as a foreign object. Multiple studies (Stanford, UCSF, others) have shown that fibroblasts, myoblasts, and mesenchymal stem cells proliferate, migrate and align on these fabricated matrices. Preclinical studies have also demonstrated that Nanoweave matrices induce remodeling phenotype, supporting the body’s regenerative repair and maintenance process.
There is increasing evidence, as shown in peer review articles, that the efficacy of tissue regeneration depends on creating a suitable micro-environment that can support cell function and decrease pathological healing. Nanoweave successfully mimics the targeted tissue, both in bio-mechanical properties and biochemical composition, and provides the appropriate cell-to-matrix interactions, adhesion, proliferation, maturation, etc.
Fibralign’s core technology provides a rich platform for scientific research and commercial development in the fields of tissue engineering and regenerative medicine. BioBridge represents just the first product commercialized using Nanoweave technology. The company’s development efforts have provided deep experience and an extensive “tool box” for application development, which has been validated in preclinical models through university research collaborations for a wide range of potential novel therapies. This translates into a compelling pipeline of future high-value products, which include novel treatments for ischemia (peripheral artery disease, myocardial infarction), advanced nerve repair, strokes, muscle regeneration and wound care.





Publications
A selection of publications related to Fibralign BioBridge® and Nanoweave® technology:
Nguyen DH, Zhou A, Posternak V, Rochlin DH. Nanofibrillar Collagen Scaffold Enhances Edema Reduction and Formation of New Lymphatic Collectors after Lymphedema Surgery. Plast Reconstr Surg. 2021 Dec 1;148(6):1382-1393.
https://pubmed.ncbi.nlm.nih.gov/34549427/
Dionyssiou, Dimitrios & Demiri, Efterpi. (2021). A comprehensive treatment algorithm for patients requiring simultaneous breast and lymphedema reconstruction based on lymph node transfer. Annals of Breast Surgery. 10.21037/abs-20-142.
Zaitseva T, Yang G, Dionyssiou D, et al. Delivery of hepatocyte growth factor mRNA from nanofibrillar scaffolds in a pig model of peripheral arterial disease. Regen Med. 2020;15(6):1761-1773. doi:10.2217/rme-2020-0023 [https://pubmed.ncbi.nlm.nih.gov/32772903/]
Hu C, Zaitseva TS, Alcazar C, et al. Delivery of Human Stromal Vascular Fraction Cells on Nanofibrillar Scaffolds for Treatment of Peripheral Arterial Disease. Front Bioeng Biotechnol. 2020;8:689. Published 2020 Jul 17. doi:10.3389/fbioe.2020.00689 [https://doi.org/10.3389/fbioe.2020.00689]
Rochlin, D, Inchauste S, Zelones J, Nguyen DH. The role of adjunct nanofibrillar collagen scaffold implantation in the surgical management of secondary lymphedema: Review of the literature and summary of initial pilot studies. Journal of Surgical Oncology, 2020. 121(1): p. 121-128 [https://onlinelibrary.wiley.com/doi/full/10.1002/jso.25576]
Inchauste S, Zelones J, Rochlin D, Nguyen DH. Successful treatment of lymphedema in a vasculopath and neuropathic patient. J Surg Oncol. 2020;121(1):182-186. doi:10.1002/jso.25590 [https://pubmed.ncbi.nlm.nih.gov/31228351/]
Rockson SG. Lymphedema after Breast Cancer Treatment. N Engl J Med. 2018;379(20):1937-1944. doi:10.1056/NEJMcp1803290 [https://pubmed.ncbi.nlm.nih.gov/30428297/]
Hadamitzky, C., Zaitseva, T. S., Bazalova-Carter, M., Paukshto, M. V., Hou, L., Strassberg, Z., et al. (2016). Aligned nanofibrillar collagen scaffolds – Guiding lymphangiogenesis for treatment of acquired lymphedema. Biomaterials 102, 259–267. doi: 10.1016/j.biomaterials.2016.05.040 [https://pubmed.ncbi.nlm.nih.gov/27348849/]
Nakayama KH, Hong G, Lee JC, Patel J, Edwards B, Zaitseva TS, Paukshto MV, Dai H, Cooke JP, Woo YJ, Huang NF. Aligned-Braided Nanofibrillar Scaffold with Endothelial Cells Enhances Arteriogenesis. ACS Nano. 9(7):6900-8 (2015). doi: 10.1021/acsnano.5b00545. Epub 2015 Jun 17.
[https://pubmed.ncbi.nlm.nih.gov/26061869/]
Huang NF, Okogbaa JN, Lee JC, Paukshto M, Zaitseva T, Cooke JP. The modulation of endothelial cell morphology, function, and survival using anisotropic nanofibrillar collagen scaffolds. Biomaterials. 34:4038-4047. (2013) [https://pubmed.ncbi.nlm.nih.gov/23480958/]
Denning D, Paukshto MV, Habelitz S, Rodriguez BJ. Piezoelectric properties of aligned collagen membranes. J Biomed Mater Res B Appl Biomater. 2014;102(2):284-292. doi:10.1002/jbm.b.33006 [https://pubmed.ncbi.nlm.nih.gov/24030958/]
Muthusubramaniam L, Peng L, Zaitseva T, Paukshto M, Martin GR, Desai TA. Collagen fibril diameter and alignment promote the quiescent keratocyte phenotype. J Biomed Mater Res A. 2012;100(3):613-621. doi:10.1002/jbm.a.33284 [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3266477/]